What is the Cost of My Varicose Vein Procedure?
Please let me know my varicose vein treatment cost. I hear this question every day in my vein clinic. Therefore, at this point, I should know the answer! However, what is really being asked is: “How much will I need to pay to have my vein procedure performed?” This question is a very different question and not an easy one to answer. Why?
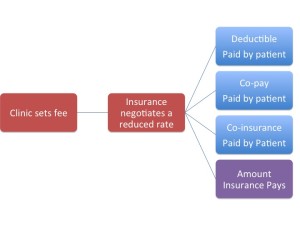
Most varicose vein procedures used to treat the rope-like, enlarged leg vessels which cause pain, swelling, itching, restless legs, skin changes and ulcers, are covered by insurance. Working through insurance companies adds to the complexities. The diagram below is a simplistic schematic of how pricing works.
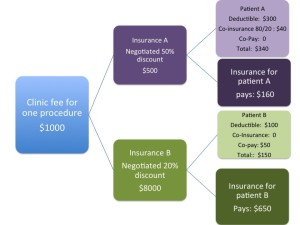
Let us look at an example with 2 patients with different insurance companies. The numbers do not reflect actual numbers, but are used to show an example.
In this example, Patient A would owe $340, Insurance pays $160 and the Medical Provider receives $500
Patient B would owe $150, Insurance pays $650 and the Medical Provider receives $800 for the same procedure
Even two people with the same insurance company may have different deductibles. They will likely have different amounts remaining on their deductible. They can also have different amounts for co-pays and co-insurance. This whole system seems unfair, not only is the medical provider receiving different sums for the same work, the patient may be paying vastly different amounts. Right now the discounted rates for each insurance company are not widely shared. If they were there would be no bargaining advantage. So as a patient, how do you get the information you need?
- Each portion of your procedure has a procedure code (CPT). Ask your medical provider which codes will be used and check with your insurance company if a pre-authorization is needed. Pre-authorization does not guarantee insurance payment, but is often required for full payment.
- Check with your insurance company. You need to know the amount remaining on your deductible. You also need to know any co-pays, and co-insurance (percentage owed by patient) that may apply to the procedures you are having done.
- Discuss payments upfront with hospital or clinic billing department. They are unlikely to give you an exact amount, as pre-authorization does not guarantee payment by insurance, but they should be able to give you a cost range
- If you are not using insurance, ask about discounts for paying cash before having your procedure.
- After your procedure, your Insurance company will send you an Explanation of Benefits (EOB). Match your bill from the medical facility with the EOB. Make sure the allowed charges and fees agree.
Do not be afraid to ask questions! We are always happy to answer your questions at Lakeshore Veins – call today! (262) 241-3999.