Open Sores on Legs That Won’t Heal — A Picture Guide
Many of us develop sores on our legs from trauma or other unknown reasons. Sometimes an open sore appears on the legs and it won’t heal. A sore is considered a non healing wound if it does not improve in 4 weeks or completely heal in 8 weeks. Non healing wounds are categorized by their underlying cause.
Most sores that won’t heal fall into 2 categories:
- Venous insufficiency ulcers
- Arterial insufficiency ulcers / diabetic ulcers
The following picture guide to open leg sores that won’t heal shows the differences in venous and arterial insufficiency ulcers. The picture guide also shows the many different appearances of venous insufficiency skin changes and open sores.
Venous Insufficiency
Venous insufficiency is by far the most common reason for open sores on the legs that do not heal. And, venous insufficiency accounts for 80-85% of non healing leg wounds. Typically, the legs swell. The swelling impairs oxygen and nutrients getting to the skin.
There are many different appearances of venous insufficiency. One appearance is that of red sores on legs. The skin is often red, scaly and itchy as in the picture below.

Venous eczema can develop in which patients develop a swollen leg with a red bumpy rash. The rash usually itches and open sores develop with scratching. Once open, the sores weep and do not heal.
Note the small red open sore and varicose veins in the picture below.
The patient below has venous eczema which is quite itchy. She scratches and causes small open sores on her anterior leg. She is much improved with compression and after venous insufficiency treatments.
The following patient has a small venous insufficiency ulcer at the ankle and itchy scaly skin with small red sores, venous eczema, all of which improved after treatment. The initial treatment for patients is usually compression.
Secondly, venous stasis skin changes are seen in patients with open sores. The skin changes can include:
- Thickening and hardening of the skin (induration)
- Redness of the skin (erythema)
- Brown discoloration of the skin – secondary to hemosiderin, which is a component of blood, leaking and staining the skin
- Lipodermatosclerosis – thickening of the skin such that there is a narrowing of the lower leg
The picture below demonstrates the brown hemosiderin staining involving most of the lower leg with an area of erythema (redness) along the anterior lower leg
The next picture shows lipodermatosclerosis with classic narrowing of the lower leg and thickening of the skin
Venous Insufficiency Ulcers
Venous insufficiency ulcers occur on the lower leg The classic location is along the inner ankle region as in the picture below. However, these open sore can also occur on the front of the shin or the lateral ankle. The pictures below shows a small sore which would not heal along the inside of the ankle. Both of these patients thought the small open sores would heal with home care. However, both required wound treatment and treatment of their underlying venous insufficiency to heal and remain healed.
There can be one or multiple venous insufficiency ulcers as in the picture below with a red open sore on the front of the leg and one near the inside of the ankle.
Typically the ulcer has irregular edges and is moist and has a clear or bloody fluid discharge. Often, the dressing over the wound may become soaked. The picture below is of an open venous stasis ulcer on the inside of the leg. This patient needed special dressings to contain the fluid leaking from the wound.
In addition, the ulcers can be small but can also be quite large. The ulcers start off as shallow ulcers however long standing ulcers and venous ulcers with secondary infection can be quite deep and involve the muscles and tendons. The picture below is of a venous insufficiency ulcer which had been present for over two years.
Venous ulcers can become infected. Signs of infection include worsening ulcer pain, increasing pus-like discharge from the wound and increasing inflammation and redness around the wound.
Arterial insufficiency Ulcers
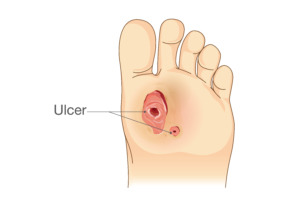
An arterial ulcer occurs because of a lack of arterial blood flow. The surrounding tissues do not get enough oxygen and the wounds do not heal. The most common risk factors for arterial ulcers are diabetes and smoking. An arterial ulcer differs from a venous ulcer. Typically an arterial ulcer involves the ball of the foot as in the diagram below or the toes or heel. Unlike a venous ulcer occurring around the ankle or lower leg. Arterial ulcers are deeper, drier and have well defined edges.
The image below is of a patient with a long standing toe ulcer. Note, the ulcer is dry and deep. Additional signs of arterial insufficiency in the leg include decreased pulses, cool limb or pain with walking.
Venous and secondly arterial insufficiency are the most common reasons for sores that won’t heal on the legs. Therefore, it is very important that you see a physician for sores that will not heal. The underlying reason for a non healing wound is determined and wound treatments are available. Additionally, it is especially important to begin treatment before other problems arise including infection. Please feel free to contact us at Lakeshore Veins, a Mequon, WI vein clinic for further questions.